Welcome, CareOregon/Health Share members! We’re glad you’re in the CareOregon and Health Share of Oregon family. CareOregon is proud to be part of the Health Share of Oregon coordinated care organization (CCO). CCOs are companies that contract with the state of Oregon to manage your health care. CareOregon is one of several insurance providers in the tri-county area that help Health Share CCO deliver care.
This page offers a brief guide to your Medicaid benefits. If you can't find what you're looking for, please call Customer Service at the numbers below, or visit our specific pages for physical health care,
dental health care, and mental health and substance use treatment.
Learn more about the Oregon Health Plan here.
Download our Easy Guide
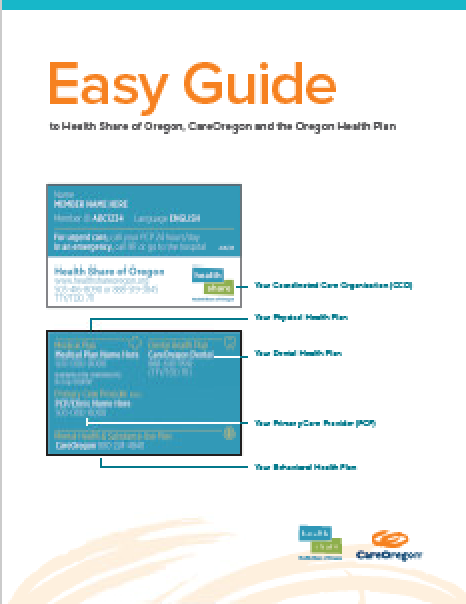 Get started with your Health Share/CareOregon benefits quickly.
Get started with your Health Share/CareOregon benefits quickly.
Download our PDF guide in the following languages: English | Spanish | Arabic | Traditional Chinese | Simplified Chinese | Russian | Somali | Vietnamese
Large print: English | Spanish | Arabic | Traditional Chinese | Simplified Chinese | Russian | Somali | Vietnamese
Click here to download the Health Share Member Handbook. If you would prefer a printed copy of the Easy Guide, call Customer Service
at 800-224-4840 or TTY 711. There’s no charge, and you’ll receive a copy within five business days. You may also receive a copy in large
print or in languages other than English.
CareOregon OHP Benefits topics
Click on a topic below to expand more information.
Complaints and Appeals
How to make a complaint or grievance
If you are unhappy with CareOregon or Health Share of Oregon, your health care services or your provider, you can complain or file a grievance at any time, for anything other than a denial of service. Your provider or authorized representative may also file a grievance on your behalf with your written consent.
We will try to make things better. You can reach out by phone or mail:
- Phone (Customer Service):
- Local: 503-416-8090
- Toll-Free: 888-519-3845
- TTY/TDD: 711
- Mail:
- Civil Rights Manager
- Health Share of Oregon
- 2121 SW Broadway, Suite 200
- Portland, OR 97201
You can also fill out a complaint and feedback form here:
CareOregon and Health Share of Oregon will work to resolve your complaint or grievance as quickly as your health condition requires. If we need more than five business days, we will send you a letter to let you know why. You will receive a final answer within 30 calendar days. We will not tell anyone about your complaint unless you ask us to.
You can also file a complaint with:
Oregon Health Authority (OHA)
Please call the OHP Client Services unit (CSU) toll free at 800-273-0557 or OHA’s Ombudsman at 503-947-2346 or toll free at 877-642-0450.
Appeals and hearings
If we deny, stop or reduce a medical service your provider has ordered, we will mail you a Notice of Action letter explaining why we made that decision. You have a right to ask to change it through an appeal and a state fair hearing. You must ask for an appeal no more than 60 days from the date on the Notice of Action letter. You can ask for a denial notice that shows a service is not covered if:
- You did not receive a written notice of denial, or;
- Your provider tells you that you will need to pay for a service that is not covered.
For full instructions on the appeals process, go to Health Share of Oregon | Appeals and Grievances
Provider Appeals
Your provider has a right to appeal for you when their physician’s orders are denied by a plan. You must agree to this in writing. Instructions for this process can be found on page 72 of your member handbook, available on the Health Share of Oregon website.
OHP Bridge program benefits
OHP Bridge is a new Oregon Health Plan (OHP) benefit package that covers adults with higher incomes. People who can get OHP Bridge must:
- Be 19 to 65 years old;
- Have an income between 139 percent and 200 percent of the federal poverty level (FPL);
- Have an eligible citizenship or immigration status to qualify; and,
- Not have access to other affordable health insurance.
Expand the section below to learn more about OHP Bridge benefits.
OHP Bridge is almost the same as OHP Plus.
The two benefit packages are almost the same. There are a few things that OHP Bridge does not cover. To learn more about what OHP Bridge does not cover, please see the table below.
| OHP Bridge covers | OHP Bridge does not cover |
|---|---|
|
|
OHP Bridge will cover adults up to age 65 who:
- Have income above traditional OHP Plus limits up to 200 percent of the federal poverty level (FPL),
- Do not have access to affordable health insurance, and
- Have an eligible citizenship or immigration status to qualify.
Income limits shown below apply through February 2025. FPL is updated annually.
| Family Size | 200% FPL |
|---|---|
| 1 | $30,120 per year |
| 2 | $40,880 |
| 3 | $51,640 |
| 4 | $62,400 |
OHP Bridge is free to members. Just like OHP Plus, OHP Bridge is free to members. That means no premiums, no copayments, no coinsurance, and no deductibles.
OHP members with income changes may be moved to OHP Bridge automatically. If you have OHP now, you don’t have to do anything to get OHP Bridge. If you report a higher income when you renew your OHP, you may be moved to OHP Bridge.
People who do not have OHP right now can apply for OHP Bridge.
Go to One.Oregon.gov to apply. You can also use that link to find information about how to apply in person, get application help, or to get a paper application. To apply over the phone, call the ONE Customer Service Center at 800-699-9075 (toll-free, all relay calls are accepted).
For more information about the OHP Bridge benefit, visit the Oregon Health Authority web page for OHP Bridge
