Pharmacy-related Star Measures
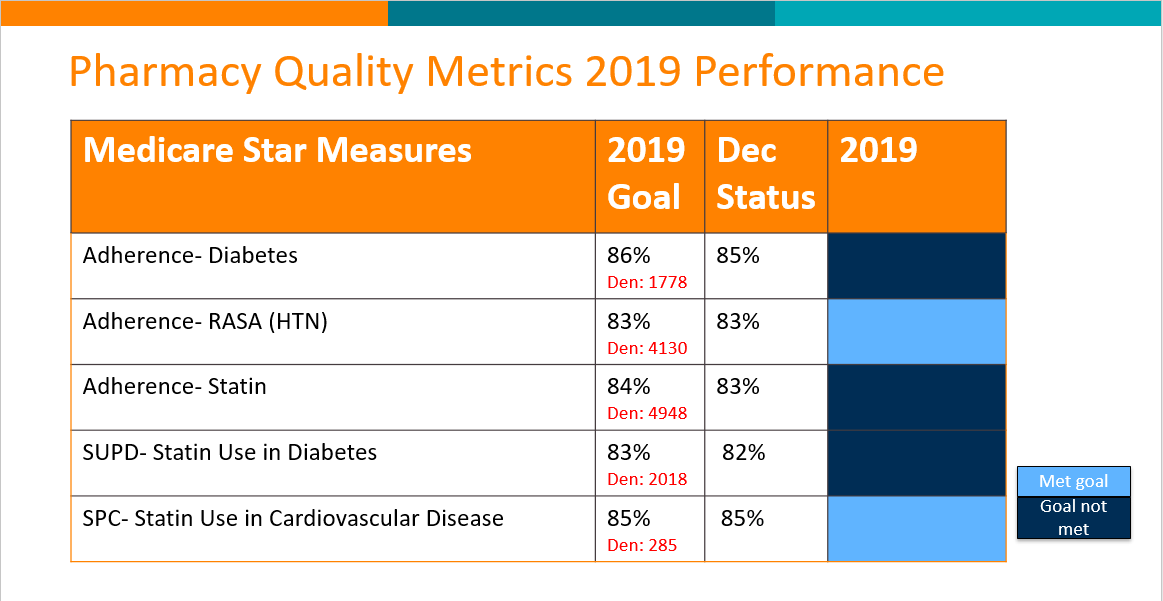
There are five main medication-related Star measures that pharmacy is focusing on: three measures on medication adherence, and two measures related to statin use. The adherence measures are for diabetes medications, renin-angiotensin inhibitors, and statins. They are measured by calculating the proportion of days covered (PDC) for each member who has received at least two fills of the medication or medication class within the measurement year. CareOregon is providing direct outreach to members taking these medications to encourage adherence by providing refill reminders, 90-day fill conversions, adherence supplies, and adherence monitoring at their community pharmacy. We are asking clinics to write 90-day prescriptions for these medications whenever possible and to assess for adherence barriers and help members overcome them. We also encourage medication synchronization, where all medications are picked up at the pharmacy on the same day.
The two statin measures are to ensure that members with diabetes or cardiovascular disease are prescribed statins. For these measures, CareOregon enlists the help of community pharmacists to close these gaps, as well as send clinics a registry of members that need statin therapy.
Click here for the Stars Pharmacy Metrics Fact Sheet.